No Mesh Hernia Repair
An Overview of an Inguinal Hernia
What is a Hernia?
More Information
Types of Inguinal Hernia
Naturally, before moving forward with an inguinal hernia repair, it is essential to determine what type of inguinal hernia you have.
Even an experienced surgeon can have difficulty determining from a physical examination what type of hernia the patient has. In that case, a standing ultrasound with a Valsalva maneuver.
The photo below represents the inguinal anatomy: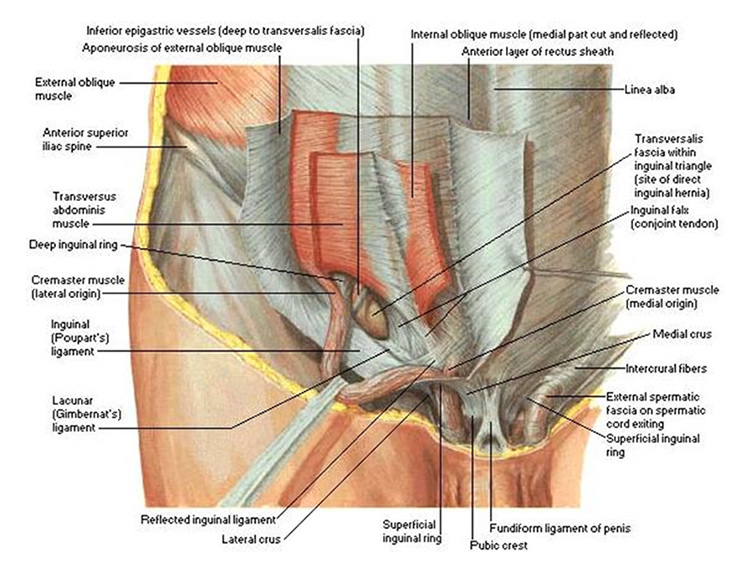
The Three Types of Inguinal Hernias
Type 1: Indirect Inguinal Hernia
The first type of inguinal hernia is an indirect inguinal hernia or sometimes called a congenital inguinal hernia. This type of hernia develops because the testicle needs a hole in the abdominal wall to allow the testicle to pop out of the pelvis and then drop down into the scrotum just before a young man is born. After the testicle passes through the hole in the abdominal wall, that natural hole is supposed close. If the hole does not close, then at a later date, the hole can dilate and allow intestines to slide out through the hole and create a bulge under the skin. On physical examination, the bulge follows the spermatic cord, and the bulge starts lateral the epigastric vessels.
Type 2: Direct Inguinal Hernia
The second type of inguinal hernia is the direct inguinal hernia or sometimes called an acquired inguinal hernia. This type of hernia develops from a tear or weakness in the floor of the inguinal canal. The damage can be a result of a sudden accident or chronic overuse. Chronic cough, difficulty with urination because of an enlarged prostate or chronic constipation are also significant risk factors. Smokers have weak connective tissue and are also at increased risk for direct inguinal hernias. The direct inguinal hernia develops in the floor of the inguinal canal medial to the epigastric vessels because this is the weakest part of the abdominal wall. On physical examination, the bulge does not follow the spermatic cord but comes straight out of the medial aspect of the inguinal floor.
Type 3: Femoral Hernia
The third type of inguinal hernia is called a femoral hernia. It occurs from a defect that is deep to the inguinal ligament. On physical examination, the bulge often appears as if it is high on the anterior medial aspect of the thigh. The bulge is usually small and difficult to palpate. A standing ultrasound may help. It is a common hernia in women.
Some patients have more than one type of hernia.
Why Differentiate Between the Types of Hernia?
It is essential to determine which type of hernia you have because each type of hernia is repaired differently. For example, patients with an indirect hernia or a congenital hernia, the muscles in the region are not damaged. There is a just natural opening in the muscles that failed to close. There is usually no need to do a full reconstruction of the inguinal floor. Often only a few sutures are required to close the hole. Direct hernias or acquired hernias are more challenging to repair because the muscles have been damaged, and thus it is harder to find healthy tissues to repair the defect. Femoral hernias develop deep to the inguinal ligament. Since most inguinal hernia repairs use the inguinal ligament to repair the inguinal floor, the standard inguinal hernia repairs will not fix a femoral hernia. So, femoral Hernias require special attention.
Why Repair a Hernia?
The primary reason to repair a hernia is if it is symptomatic. Hernias often cause significant pain. Exercise and long periods of standing can be strenuous. Athletes often have difficulty performing at 100% and are no longer competitive. Intercourse can be painful. Also, the bulge can increase in size to the point that it is easily visible through clothes and thus becomes an embarrassment.
The most serious problem with a hernia occurs if the intestines get stuck (incarcerated) in the hernia. Luckily, this is rare. But when it does happen, incarcerations require an emergency operation. Indirect inguinal hernias and femoral hernias have a higher risk of incarceration than direct inguinal hernias. Another reason to repair a hernia is if you travel to countries with inadequate medical care. Asymptomatic hernias do not require repair.
When to Repair a Hernia?
Inguinal hernias and femoral hernia are only dangerous if your intestines become incarcerated (i.e., the intestines become trapped in the hernia). On the other hand, the chance for incarceration is rare. So, in most situations, hernia repair can be delayed until you’re in optimal health or at a time most convenient for you. Also, I advise for repair before traveling to a third world country.
Hernia Repair With Mesh or No Mesh?
There are two basic methods to repair a hernia. The first method uses sutures to repair the hernia through an incision. The second method of repair involves placing a piece of mesh to patch the hole. The mesh can be placed on the deep side of the hernia using a laparoscope, or the mesh can be placed to cover the outside of the hernia using an incision.
The argument for a hand-sewn repair (i.e., no mesh), is that there is no foreign body placed in the body. It is common for people to develop scar tissue around the mesh. This fibrosis causes the mesh to become stiff and hard. Then when you bend and twist, and the mesh does not bend and twist with you, the sheer stresses causes pain. Sometimes one of the nerves or spermatic cord gets stuck to the mesh, and severe pain can result. Then exercise becomes impossible because of pain, and ejaculation causes a severe burning sensation in the spermatic cord and testicle. Chronic pain after mesh hernia repairs affects 15% of patients. A significant number of those patients with pain have to have the mesh removed with another operation. Even after removing the mesh, the patient is often only about 80% better. Most Surgeons argue for the use of mesh because of the lower recurrence rate. But their argument is flawed. If you look at the numbers, the chance for a recurrent hernia after a mesh repair is 3%. The chance for a recurrent hernia after a non-mesh repair is about 4%. But to achieve this 1% lower recurrence rate the patient runs about a 16% chance of chronic pain.
I strongly feel that since the risk of chronic pain from the mesh is so much higher than the recurrence rate that the best hernia repair is the suture repairs. No Mesh!
The Types of Non-Mesh Hernia Repairs
There are many methods for Pure Tissue Repair. The following describes the most common and proven techniques.
Bassini: There are numerous ways to repair an inguinal hernia with the local tissue. The Bassini technique repairs the inguinal floor by sewing together the transversalis fascia and the inguinal ligament. Then the external oblique is repaired over the spermatic cord. The Bassini is a classic technique that has been perfected over the last hundred years. The repair has excellent results.
Shouldice: The Shouldice hernia repair involves using a running suture to first plicate and strengthen the inguinal floor. And then a second running suture is used to plicate and the oblique muscles. The Shouldice results in a four-layer repair. There is minimal tension in the suture line. The recurrence rate for the Shouldice repair is equal to or better than the mesh repairs. Shouldice is an excellent technique for hernia repair.
Marcy: The Marcy hernia repair is excellent for indirect hernias. It involves separating the hernia sac from the spermatic cord. Then tying off hernia sac or inverting the hernia sac into the retroperitoneal space. The internal ring is then tightened with a few sutures. The external oblique aponeurosis is closed. There is no tension on the repair. The post-operative pain is minimal, and there is a quick recovery. The results are excellent.
The Desarda: The Desarda hernia repair uses the external oblique aponeurosis as a patch to reinforce and repair the inguinal floor. (Note: this is similar to mesh hernia repairs, but your tissue is used instead of plastic.) The remaining sections of the external oblique aponeurosis are closed over the spermatic cord and to finish up the repair. The results are excellent. The recurrence rates are low. There is minimal tension on the repair.
McVay: The McVay hernia repair has been used by surgeons for over 50 years. The McVay hernia repair is unique in that it uses the Cooper’s Ligament instead of the inguinal ligament to repair the inguinal floor. For example, with the Bassini repair, the transversalis is sewn to the inguinal ligament. But in the McVay repair, the transversalis fascia is sewn to Cooper’s ligament medially and then to the inguinal ligament laterally. The McVay repair is beneficial in situations where the inguinal ligament is weak or absent. And it is the preferred method when a femoral hernia is present. There can be a moderate amount of tension on the repair. And often a relaxing incision is required.
Which Type of Hernia Repair is the Best?
Each hernia repair needs to be tailored to the patient’s anatomy and needs. Your surgeon should have all these various methods available and then choose which will give the best result for your situation. For example, in a young athlete with an indirect inguinal hernia, the Marcy hernia repair with ringplasty yields excellent results with minimal dissection and minimal postoperative pain.
For direct inguinal hernias, the Bassini, the Shouldice, and the Desarda are all excellent choices. The Bassini repair is a great technique, especially if the floor of the inguinal canal is just weak and not fully torn. The traversalis fascia is sewn to the shelf of the inguinal ligament. The Desarda also provides excellent results. There is very little tension on the repair. But the Desarda repair does require a strong external oblique aponeurosis to serve as a patch. Therefore, it is not a good option if the external oblique aponeurosis is torn or weak. Shouldice is an excellent operation. There little tension on the repair. The four-layer repair is solid. But it does rely on an intact inguinal ligament. Thus, there will be times when the Shouldice may not be possible.
The McVay repair involves the use of Cooper’s ligament instead of the inguinal ligament to repair the inguinal floor. It is an especially useful technique in situations in which the inguinal ligament is damaged, or there is an associated femoral hernia. The McVay hernia repair does have tension on the repair and may require more recovery time.
Your surgeon should know all of these techniques for hernia repair. And he or she will often find that a hybrid operation using the best ideas from each method are needed to achieve the best result.
Muscle and Nerves
Cremasteric Muscle: The cremasteric muscle starts at the internal inguinal ring and runs down to the testicle. During intercourse and when cold, the cremasteric muscle contracts and pulls the testicle up. But the cremasteric muscle can add a significant amount of bulk to the spermatic cord. Some surgeons routinely advise removing the cremasteric muscle to make the spermatic cord smaller and thereby allowing a tighter closure of the internal ring. But then the testicle will not rise and fall as it should. Also, important blood vessels and nerves travel with the cremasteric muscle. Dr. Brown does not want to compromise the testicle in any way, and therefore does not remove the cremasteric muscle.
Nerves: There are three major nerves in the inguinal area. The iliohypogastric nerve, the ilioinguinal nerve, and the genital nerve. The iliohypogastric nerve provides sensation to the pubic hair area and the upper part of the scrotum or Mons. The ilioinguinal nerve provides feeling to the inguinal ligament, on the inside of the upper thigh, and the outside of the scrotum or Mons. The genital nerve provides innervation to the cremasteric muscles and the testicle or labia majora. Damage to any of these nerves can cause chronic pain after the surgery. Some surgeons advise routine transection of these nerves to avoid postoperative pain. But cutting the nerves causes the skin to be numb. And if the damaged nerve forms a neuroma, then the patient suffers allodynia. Dr. Brown feels it is best to carefully identify the nerves during the operation. And then he takes care not to damage the nerves. The iliohypogastric nerve runs parallel to the inguinal ligament and deep to the external oblique aponeurosis. It will emerge through a hole in the external oblique aponeurosis just above the external inguinal ring and continue its journey to the skin.
The ilioinguinal nerve joins the spermatic cord (or round ligament in women) at the internal inguinal ring and then runs along the anterior superior aspect of the spermatic cord (or round ligament). The genital nerve usually joins the spermatic cord (or round ligament) at the internal inguinal ring. It then runs along the posterior aspect of the spermatic cord (or the round ligament). Of the three nerves, the course of the genital nerve is the most variable. Instead of traveling with the spermatic cord (or round ligament), it can be found near the inguinal ligament or running along the floor of the inguinal canal.
Additional Resource
Haastrup E, Andresen K, Rosenberg J. Low reoperation rates in young males after sutured repair of indirect inguinal hernia: Arguments for a tailored approach. Am J Surg. 2017 Mar 14. pii: S0002-9610(16)30782-6.
https://www.ncbi.nlm.nih.gov/pubmed/28391976
Note: Suture repairs are excellent in young males.
Gedam BS, Bansod PY, Kale VB, Shah Y, Akhtar M. A comparative study of Desarda’s technique with Lichtenstein mesh repair in treatment of inguinal hernia: A prospective cohort study. Int J Surg. 2017 Mar;39:150-155.
https://www.ncbi.nlm.nih.gov/pubmed/28131917
Note: Suture repairs are as good as mesh repairs.
van Kerckhoven G, Toonen L, Draaisma WA, de Vries LS, Verheijen PM. Herniotomy in young adults as an alternative to mesh repair: a retrospective cohort study. Hernia. 2016 Oct;20(5):675-9.
https://www.ncbi.nlm.nih.gov/pubmed/27522362
Note: Suture repairs have excellent results.
Pogorelić Z, Rikalo M, Jukić M, Katić J, Jurić I, Furlan D, Budimir D, Biočić M. Modified Marcy repair for indirect inguinal hernia in children: a 24-year single-center experience of 6826 pediatric patients. Surg Today. 2017 Jan;47(1):108-113.
https://www.ncbi.nlm.nih.gov/pubmed/27170378
Note: Excellent results with Marcy repair.
Iakovlev V, Koch A, Petersen K, Morrison J, Grischkan D, Oprea V, Bendavid R. A Pathology of Mesh and Time: Dysejaculation, Sexual Pain, and Orchialgia Resulting From Polypropylene Mesh Erosion Into the Spermatic Cord. Ann Surg. 2017 Jan 6
https://www.ncbi.nlm.nih.gov/pubmed/28067674
Note: damage to the spermatic cord from mesh.
Verhagen T, Loos MJ, Scheltinga MR, Roumen RM. Surgery for chronic inguinodynia following routine herniorrhaphy: beneficial effects on dysejaculation. Hernia. 2016 Feb;20(1):63-8.
https://www.ncbi.nlm.nih.gov/pubmed/26260489
Note: Sexual dysfunction after mesh hernia repair.
Hakeem A, Shanmugam V. Inguinodynia following Lichtenstein tension-free hernia repair: a review. World J Gastroenterol. 2011 Apr 14;17(14):1791-6
https://www.ncbi.nlm.nih.gov/pubmed/21528050
Note: Pain after mesh repair.
Nikkolo C, Lepner U. Chronic pain after open inguinal hernia repair. Postgrad Med. 2016 Jan;128(1):69-75. doi: 10.1080/00325481.2016.1121090.
https://www.ncbi.nlm.nih.gov/pubmed/26567717
Note: Pain after mesh repair.
Goltsman D, Munabi NC, Ascherman JA. The Association between Smoking and Plastic Surgery Outcomes in 40,465 Patients: An Analysis of the American College of Surgeons National Surgical Quality Improvement Program Data Sets. Plast Reconstr Surg. 2017 Feb;139(2):503-511.
https://www.ncbi.nlm.nih.gov/pubmed/28121897
Note: Smoking and healing.
Contact Us
M-F 9am – 5pm
15965 Los Gatos Blvd. Suite 201
Los Gatos, CA 95032
PHONE: 408.358.1855
FAX: 408.356.4183
